Last Updated on January 14, 2021
Contents
What is ICSI?
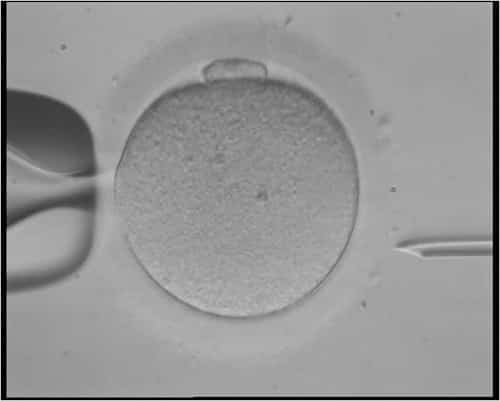
ICSI (intracytoplasmic sperm injection) is a simple process on the surface. Embryologists performing ICSI use a small, glass tool called a pipette to inject a single sperm into a single egg. Fertility doctors recommend and use IVF with ICSI when the risk of IVF failure is high due to issues with sperm quantity or quality, egg quantity or quality, or a combination of factors.
Successful IVF treatment requires two important events: fertilization and implantation. Fertilization usually occurs several hours after a sperm penetrates an egg. Under normal IVF circumstances, fertility specialists mix sperm with an egg in a dish, and allow time for fertilization to occur. Unfortunately, in a small amount of IVF cases, fertilization does not occur.
Injecting sperm directly into the egg increases the chances of fertilization where it would otherwise be extremely difficult or impossible.
Why Does One Get ICSI?
The specific situations when an ICSI is being considered is when there is:
- Male infertility
- A low sperm count
- Poor sperm movement,
- The sperm is shaped abnormally
- You underwent an IVF before
- Your treatment involves the use of frozen sperm of low quality
- Your sperm needs to be surgically collected due to either a blockage that doesn’t allow sperm to reach the ejaculation or due to a vasectomy
There are situations when males undergo this procedure even when it’s not necessary, simply to increase their chances. A man should also consider ICSI if he’s had a vasectomy reversal. The reason is the fact that sperm antibodies may be the culprits when it comes to fertilization failure.
However, if there is no evidence that the male is infertile, then it will be difficult to get an ICSI.
Male infertility contributes to about 20% of all infertility cases (approximately 1 in 5 infertile couples). In male infertility factor cases, sperm cannot or do not successfully fertilize eggs, due to one or more issues.
Low sperm count makes up the majority of male infertility factor cases. Sometimes, the testes simply do not produce enough sperm for pregnancy. Other times, blockages and other transport issues (including vasectomy) make pregnancy difficult or impossible.
IVF normally requires large numbers of motile, healthy sperm. The sperm collected in the IVF process must be able to reach the egg and permeate the egg’s membrane in a certain amount of time. If the male’s sperm count is too low, the chances of IVF success drop dramatically. Similarly, low sperm motility significantly reduces chances of fertilization.
IVF with ICSI improves chances of success by removing the barriers to fertilization caused by male infertility. With this process, fertility specialists require fewer sperm, and can around issues of low sperm motility.
IVF with ICSI Benefits
ICSI increases the chance of success with IVF in specific couples and situations. As discussed above, it makes pregnancy possible in situations where male fertility prevents it, including:
- Low sperm count
- Low sperm motility
- Blockages/sperm transport issues
- Multiple failed IVF cycles
- Low egg count or poor egg quality
Furthermore, the IVF with ICSI benefits go beyond male infertility factor and egg quantity or quality issues. Men who’ve had a vasectomy generally cannot produce offspring unless it’s reversed. With ICSI, however, fertility specialists can use the male’s sperm (which are still being produced) to fertilize the eggs. Other situations include paralysis or a physical defect that impacts sex, ejaculation, sperm production, or another male reproduction issue.
Egg Quality Issues. Directly injecting sperm can also improve IVF success in cases with a low number of viable, healthy eggs, or poor egg quality. Sometimes referred to as “egg factor,” these issues lower the chances of success with IVF. When fertility doctors use ICSI with IVF, sometimes, the risks that egg factors pose can be mitigated or eliminated.
What is the process?
ICSI differs from IVF in one primary way. With IVF, fertility doctors mix many sperm together in a dish with a viable, healthy egg. Typically, a healthy sperm then permeates the lining of the egg and fertilizes it.
But with direct sperm injection, the fertilization process is more straightforward. Embryologists “help” sperm fertilize the eggs by placing them directly inside the egg.
- First, the fertility clinic collects sperm and retrieves eggs on the same day. Or, the clinic thaws frozen eggs, sperm, or both.
- After sperm collection and egg retrieval, an embryologist selects a sperm, and then injects that sperm directly into the egg, using a glass pipette (similar to a hollow needle). Ideally, the sperm and egg together become an embryo.
- The embryologist repeats the process for every egg.
Even if the male partner in a couple produces a small number of sperm, embryologists can successfully perform ICSI.
This process improves chances of fertilization, but does not guarantee fertilization. After fertilization, the eggs must divide into four to eight cells and become embryos before they can be transferred back into the uterus. That process takes approximately 3 days, but can take as few as two days.
When couples choose IVF with ICSI, the embryologist performs the work the same day the sperm and egg are retrieved. Similarly to IVF, couples can choose to use donor sperm or their own, or donor eggs or their own.
If the sperm count in the ejaculate is too low or is non-existent, a specialty clinic can extract sperm using a process called Testicular Sperm Extraction (TESE).
IVF with ICSI Risks and Side Effects
The process poses some serious risks that could impact pregnancy or the baby. For example, if an unhealthy sperm fertilizes the egg, the baby is at risk for abnormalities.
Risk of Multiples – Lower than IVF without ICSI
While IVF generally increases risk of multiples, ICSI reduces the chances of having multiple births. In fact, research shows that directly injecting sperm into eggs resulted in more singleton births than multiples. With this process, a single sperm fertilizes a single egg, and generally, the single embryo is transferred. There is a small risk of the embryo dividing and resulting in identical twins. Without it, multiple eggs may be fertilized.
Note, however, that with or without ICSI, if multiple embryos are transferred, a woman could become pregnant with multiple babies.
If a woman does become pregnant with multiples, risks include:
- Premature delivery
- Low birth rate
- Difficult pregnancy
- Higher blood pressure
- Gestational diabetes
Risks to Embryos
The process of injecting sperm using a needle, through the lining of the egg creates some risk of damage to embryos in IVF with ICSI. Unfortunately, some eggs become damaged, but “approximately 90% of the eggs injected survive” (Source). Most likely, an embryologist will fertilize multiple eggs with sperm and therefore increase the chances of having a viable embryo to transfer.
Risks of Birth Defects
The risk of having a baby with birth defects after using IVF with ICSI is minimal, at less than one percent. The potential birth defects include:
- Chromosome abnormalities
- Hypospadias
- Angelman syndrome
- Beckwith-Wiedemann syndrome
- Physical disabilities (especially around male genitals)
Why does ICSI pose a risk of birth defects? The primary reason is that IVF with ICSI as a process boosts the chances of fertilizing the egg, but does not necessarily require healthy sperm to do so. It simply improves fertilization and does not rule out the possibility of birth defects.
With natural fertilization, the healthiest sperm tend to fertilize the eggs, while unhealthy, slow sperm do not. In other words, natural fertilization allows for the natural selection process to do its work of ensuring only the strongest and best sperm produce offspring.
ICSI ultimately removes the natural selection process and in doing so, creates risk in IVF treatment. It increases the chance of birth defects by giving potentially unhealthy sperm a chance to fertilize the egg. The risks most commonly associated include physical abnormalities or disabilities. An article published on healthcentre.org.uk
suggests the risk could be as high as 4.2% of births resulting in a major disability.
Before choosing ICSI, discuss the risks with a fertility specialist. Always ask about potential risks and side effects, given your specific infertility situation, rather than general risks.
How much does ICSI cost?
Costs vary by fertility clinic and location. On average, the process costs around $1,500. You can use an IVF cost calculator to determine the cost of IVF with ICSI. This is an additional, separate cost and may not be covered by insurance.
Read more: ICSI Success Rates
References
- Embryo transfer and multiple births (http://www.hfea.gov.uk/2587.html#3047)
- Advantages ICSI Disadvantages of ICSI (http://www.healthcentre.org.uk/fertility-treatment/icsi.html)
- Stages of the IVF Process | ICSI Procedure | The Bridge Centre (http://www.thebridgecentre.co.uk/fertility_treatments/IVF_ICSI_treatment_stages)
- Male Infertility – Symptoms, Causes, Diagnosis, Treatment (https://www.andrologyaustralia.org/your-health/male-infertility/)
- Male Infertility – Mayo Clinic (http://www.mayoclinic.org/diseases-conditions/male-infertility/basics/tests-diagnosis/con-20033113)
- ICSI-IVF: Risks, What to Expect, and Success Rates (https://www.verywell.com/what-you-should-know-about-icsi-ivf-1960209)